Background: The prognosis of relapsed/refractory (R/R) acute myeloid leukemia (AML) remains poor; therefore, novel treatment strategies are required urgently. Meanwhile, recent clinical trials have demonstrated that CAR-T cells for AML have been less successful than those targeting CD19 for B cell malignancies. Recently, we developed piggyBac-modified ligand-based CAR-T cells that target CD116, also called granulocyte-macrophage colony-stimulating factor (GM-CSF) receptor (GMR) α chain, for treating juvenile myelomonocytic leukemia (Nakazawa, et al. J Hematol Oncol. 2016). Since CD116 is overexpressed in 60%-80% of AML cases, the present study aimed to develop a novel therapeutic method for R/R AML using GMR CAR-T cells.
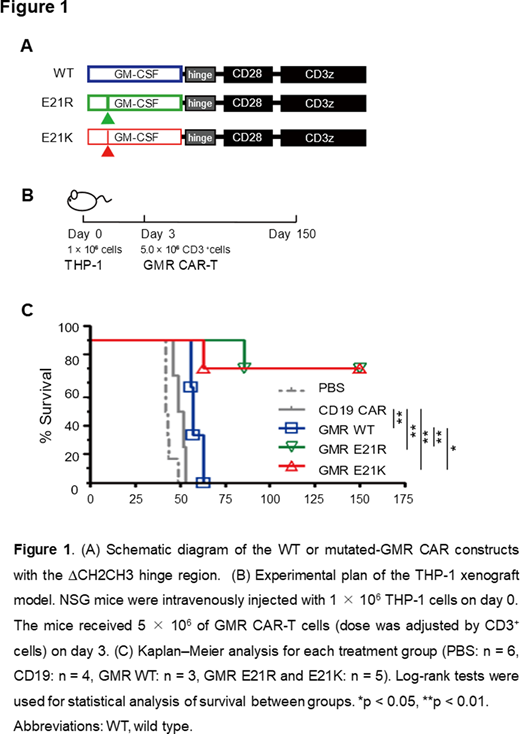
Methods: CD116 expression in AML cell lines or primary leukemia cells were examined using flow cytometry. The original piggyBac transposon plasmid for GMR CAR comprises GM-CSF as an antigen recognition site, IgG1 CH2CH3 hinge region, CD28 costimulatory domain, and CD3ζ chain. To improve the in vivo persistency and anti-tumor effects, two types of spacer (∆CH2H3 and G4S) that lack CH2CH3 lesion were newly constructed. In order to modulate the antigen recognition ability, mutated ligand-based GMR CAR vectors were constructed with a mutation at residue 21 of GM-CSF that is reported to play a critical role in its biological activity (Lopez, et al. Embo j. 1992). All the GMR CAR-T cells were generated with piggyBac gene modification. To investigate the in vitro anti-tumor activity, GMR CAR-T cells were co-cultured with AML cell lines. In order to evaluate the in vivo anti-tumor effects, NOD.Cg-PrkdcscidIl2rgtm1Wjl/SzJ (NSG) mice were intravenously injected with THP-1, THP1-ffLuc, or MV4-11 and then treated with GMR CAR-T cells. To characterize the safety profile of GMR CAR-T cells, peripheral blood mononuclear cells or polymorphonuclear cells were co-cultured with GMR CAR-T cells at an effector:target ratio of 1:1 for 3 days. Thereafter, B cells, NK cells, neutrophils, and monocytes were quantified using flow cytometry using counting beads.
Results: Approximately 80% of the AML cells predominant in myelomonocytic leukemia expressed CD116. PiggyBac-modified GMR CAR-T cells displayed a favorable CD45RA+CCR7+-dominant phenotype, consistent with our previous findings. GMR CAR-T cells exhibited potent cytotoxic activities against CD116+ AML cells in vitro. GMR CAR-T cells incorporating a G4S spacer significantly improved the long-term in vitro and in vivo anti-tumor effects as compared to those incorporating a ∆CH2CH3 spacer. Furthermore, by employing a mutated GM-CSF at residue 21 (E21K and E21R) as an antigen recognition site, the in vivo anti-tumor effects were also substantially improved along with prolonged survival (Figure 1) over controls (PBS or CD19.CAR-T cells) (all, p < 0.01) as well as over GMR CAR-T cells with a wild-type GM-CSF ligand (E21R: p < 0.01; E21K: p = 0.02), with 4 out of 5 mice surviving for > 150 days. Safety tests revealed that the toxicity of GMR CAR-T cells was restricted to normal monocytes. It is noteworthy that the cytotoxic effects of GMR CAR-T cells on normal neutrophils, T cells, B cells, and NK cells were minimal.
Conclusions: GMR CAR-T cell therapy appears to be a potentially useful strategy for CD116+ R/R AML. Based on the promising results, we plan to perform the first-in-human clinical trial of GMR CAR-T cells.
Saito:Toshiba Corporation: Research Funding. Hasegawa:Toshiba Corporation: Research Funding. Inada:Kissei Pharmaceuticals: Ended employment in the past 24 months. Nakashima:Toshiba Corporation: Research Funding. Yagyu:Toshiba Corporation: Research Funding. Nakazawa:Toshiba Corporation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal